Opportunity knocks
Healthcare is an obvious sector to deploy AI in. It generates tsunamis of data, vast amounts of money are spent on it, and there are plenty of opportunities to improve the quality of its products and services by making them more intelligent and intelligible.
It is a mistake to think of healthcare as a single monolithic entity. Will Smart is the former CIO for the NHS in England, and he points out that healthcare carries out the activities of numerous different industries, including hotels, catering, research, professional services, janitorial services, logistics, manufacturing, and many others.
What kinds of AI should healthcare managers be looking into? Robotic process automation (RPA) is one of the three strands of AI making most headway beyond the tech giants. (Much RPA does not involve AI, but increasingly, some of it does.) The healthcare services of most countries are large, bureaucratic enterprises, so RPA would be an obvious application. But Smart says you would struggle to find many healthcare organisations which are embracing RPA. It could enhance efficiency, but it is not shiny and exciting, and it won’t cure cancer.
Diagnostics
Alongside RPA, the other two applications of AI which are most consistently being piloted and rolled out at scale today are chatbots and analytics. Chatbots are less common in most healthcare systems than you might expect, but various kinds of analytics are being widely trialled in diagnostics. Hardly a day goes by without a new paper reporting that machines have proved themselves more capable at diagnosing some malady or other than human doctors or radiologists.
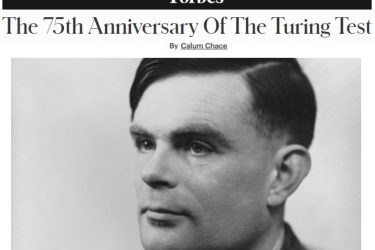
This has naturally led to speculation about machines taking the jobs of human medical staff, especially radiologists. Back in 2016, Geoff Hinton, often described as the father of deep learning, said “If you work as a radiologist, you’re like the coyote that’s already over the edge of the cliff, but hasn’t yet looked down so doesn’t realise there’s no ground underneath him. People should stop training radiologists now. It’s just completely obvious that within five years, deep learning is going to do better than radiologists.”
Hinton’s enthusiasm was premature. Gary Marcus is a prominent skeptic about deep learning, and he says, “the number of radiologists who have been replaced by AI systems to date is approximately zero”. Today, deep learning diagnostic systems are brittle, and less versatile than we need them to be. But this could well be an example of Amara’s Law: we often over-estimate the impact of a technology in the short term and under-estimate it in the longer term. Ed Kessler is commercial director of cfes, a provider of healthcare infrastructure and clinical support services, and he thinks Hinton might be proved right in fifteen years or so.
Change is hard
Change does not come easily in healthcare. There are numerous powerful vested interests, and there is often no effective market to encourage innovation and drive efficiency. In 2013, Johnson & Johnson secured FDA approval for an automated anaesthetic system called Sedasys for use in relatively unchallenging procedures like colonoscopies. It carried out thousands of successful operations in Canada and the USA, but the profession fought back, and sales were sluggish, even though the machine cost $150 per operation, whereas a human anaesthetist cost $2,000. A few years later, J&J exited the business.
The eminent American cardiologist, scientist and author Eric Topol accuses his colleagues in the medical profession of condescension towards their patients. He thinks too many doctors are parsimonious with the information they glean about our health, on the grounds that a little knowledge is a dangerous thing. His 2015 book, “The Patient Will See You Now” calls for a role reversal, in which the “medical deity” (the MD) is overthrown, and the patient becomes the CEO of their own healthcare. The sub-title of his 2019 book, “Deep Medicine”, encapsulates his view of a hopeful future: “How Artificial Intelligence Can Make Healthcare Human Again”.
Medical AI in consumer devices
Topol and others think that developments in consumer technology could impose change on the medical profession. Apple Watches can already check your heart rate, perform an electrocardiogram test, and check for atrial fibrillation. Cheap and simple sensors attached to watches and smartphones – and later, smart glasses, will sample our sweat and our blood glucose. Our breath will be sampled and digitised, and used to detect cancer, or potential heart problems. Our phones’ cameras will scan for skin cancers, and their microphones will capture data about our voices to assess our mood, or diagnose Parkinson’s disease, or schizophrenia.
Within a decade, we may have as many sensors constantly monitoring our well-being as a Formula One car. At first, doctors may complain of being inundated by irrelevant data from the “worried well”, but the signal will increasingly be analysed for them by AI in our devices and in the cloud. Soon, Topol thinks, doctors will welcome the greatly improved picture of their patients the devices afford, and they will come to accept the ability and inclination of patients to take on some of the responsibility for their own healthcare.
Democratised and decentralised
Much more immediately, the covid-19 pandemic is likely to leave a lasting imprint on the medical profession. Will Smart says that 40% of UK doctors appointments are now being handled by phone or video calls. Admittedly, this saves more time for the patient than it does for the doctor, but the longer the disease lingers, the harder it will be to go back to old ways. Telemedicine opens the door for more AI, for instance in triage, with chatbots determining how urgently a patient dialling in needs to be seen, and by which professional.
Medicine could become decentralised by AI as well as democratised. Acute hospitals are the fixed points in most healthcare systems today. They are based on a Napoleonic model established to bring specialists together, and facilitate large capital expenditure. But it is an open secret that healthcare is responsible for as little as 20% of a patient’s well-being. The rest is dependent on income, employment, marital status, etc. Doctors have spent the last two centuries getting more specialised, and AI could enable them to become generalists again. As AI-infused devices become smaller, more intelligent and more intelligible, doctors can take a more rounded view of their patients, relying on their devices to diagnose particular ailments accurately.
Will Smart and some colleagues are developing a medical assistant which sits in the doctor’s pocket, transcribing patient conversations, pulling up medical records, creating clinical notes and making suggestions. Siri is getting sexy.